
In the latest edition (DSM-V), alcohol dependence and abuse have been replaced by a single disease. The diagnostic criteria for alcohol-use disorder (AUD) have also evolved with each iteration of the DSM. This is especially critical and timely because the latest estimates using the DSM-V diagnostic criteria indicate that the current past year PTSD prevalence was 4.7% and the lifetime prevalence rate was 8.3 (Kilpatrick 2003). These revisions to the diagnostic criteria of PTSD are largely evidence-based and have helped to stimulate a much-needed increase in research directed at this debilitating disorder.

Individuals suffering from these disorders often re-experience a previously traumatic event, make significant efforts to avoid internal or external reminders of the trauma and exhibit hyperarousal in response to relatively neutral stimuli.

The diagnostic criteria of PTSD include four clusters of symptoms: intrusion, avoidance, negative alterations in cognitions and mood and alterations in arousal and reactivity ( Guina et al.
Revisions to the diagnostic criteria of PTSD continued until the latest edition of the DSM (DSM-V) which recognized that, although anxiogenic symptoms are a cornerstone of PTSD, this disease is better described by a new category of mental illnesses, termed trauma- or stressor-related disorders, in which exposure to a traumatic or otherwise adverse environmental event precedes the onset of each disorder. This change was prompted by the acknowledgment that the etiological agent that triggered the symptoms was outside the afflicted individual rather than merely a reflection of some personal weakness or failing, a realization that slowly began to reduce the stigma associated with this disorder. This term replaced other labels such as ‘shell shock’ and ‘war neurosis’ that had appeared in the literature for hundreds of years ( Crocq & Crocq 2000 Trimble 1985).
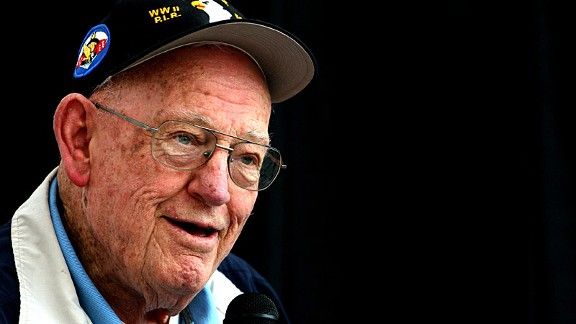
Lt buck compton ptsd manual#
It has long been recognized that exposure to traumatic events can elicit, in some individuals, the emergence of a spectrum of debilitating and enduring anxiety-related symptoms, but the term post-traumatic stress disorder (PSTD) was not officially recognized as an anxiety disorder until the 3rd edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III).
Lt buck compton ptsd trial#
We conclude by discussing key gaps in our knowledge and strategies for addressing them: in particular, we (1) highlight the need for better animal models of the comorbid condition and better clinical trial design, (2) emphasize the need for examination of subpopulation effects and individual differences and (3) urge cross-talk between basic and clinical researchers that is reflected in collaborative work with forward and reverse translational impact. We also review animal models that aim to examine comorbid PTSD and AUD, highlighting where the models parallel the human condition, and we discuss the strengths and weaknesses of each model.

We summarize epidemiological data documenting the prevalence of this comorbidity, review what is known about the potential neurobiological basis for the frequent co-occurrence of PTSD and AUD and discuss successes and failures of past and current treatment strategies. The goal of this review is to summarize the current state-of-the-science on comorbid PTSD and AUD. Although we have some understanding of the structural and functional brain changes that define each of these disorders, and how those changes contribute to the behavioral symptoms that define them, little is known about the neurobiology of comorbid PTSD and AUD, which may be due in part to a scarcity of adequate animal models for examining this research question. Post-traumatic stress disorder (PTSD) and alcohol-use disorder (AUD) are highly comorbid in humans.


 0 kommentar(er)
0 kommentar(er)
